
06 Nov Knee joint injections in Singapore: a quick, minimally invasive option to get you moving again
By Dr Gerard E.E., MBBS, MRCS, DP Dermatology — aesthetic dermatologist with a special interest in longevity medicine, sports medicine and orthopaedics; published under “Gerard EE” on PubMed.
Introduction
If knee pain is boxing you into shorter walks, fewer stairs and cancelled plans, a targeted injection into the joint can be a fast, clinic based way to break that cycle without surgery. In my Singapore practice I offer corticosteroid, hyaluronic acid (“gel shots”), platelet rich plasma (PRP) and bone marrow aspirate concentrate (BMAC). Used thoughtfully, these treatments create breathing room from pain so you can return to the rehabilitation that builds durable capacity. For readers new to injections—and for those already considering them—this article explains where injections fit, who tends to benefit, what I do procedurally, and what honest results look like in the real world.

Who this article is for
This guide is written for patients in Singapore who are exploring intra articular knee injections for the first time or are weighing them against other options. My aim is to give you a clear, evidence aware overview in plain language so you can make an informed choice with your clinician.
When injections fit into care (and when they do not)
Injections are not a first stop, and they are not magic. Most people begin with physiotherapy, activity modification, simple medicines and weight management where relevant. When pain still blocks life or rehabilitation despite those steps, an injection can reset the playing field. In my experience, the best candidates are people with mild to moderate osteoarthritis without major deformity. Those with severe, deforming arthritis rarely find injections match their expectations, and I will say that upfront so we can plan the right pathway together. Guideline bodies echo this framing: they emphasise shared decision making, judicious use of corticosteroid for short term relief, caution about routine hyaluronic acid, and an evidence base for PRP that is promising but still method dependent.
How the options work
It helps to picture the knee as a machine that relies on good “oil.” Your knee’s synovial fluid lubricates, cushions and cools the moving parts. Osteoarthritis makes that “oil” thin and gritty. Different injections address different levers—reducing inflammation, improving lubrication or nudging the joint’s biology—to help you move with less pain.
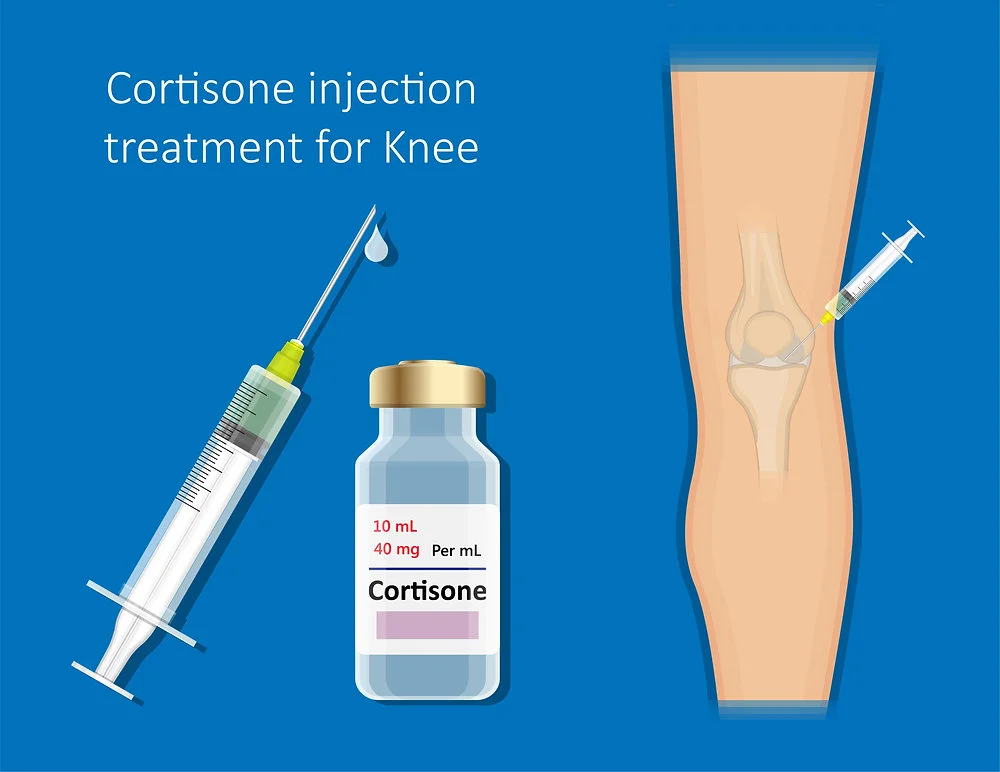
Corticosteroid
Corticosteroid is my go to when the joint is hot and irritable and fast relief matters. It often calms pain within days to a week, but its benefit is usually measured in weeks to a few months. I am conservative about repeating steroids frequently because a high quality randomised trial of triamcinolone every three months for two years showed more cartilage loss than placebo without superior long term pain control. That finding does not banish steroids, but it does shape how carefully and sparingly I use them.
Hyaluronic acid (“gel shots”)
Hyaluronic acid aims to restore lubrication. In Singapore I commonly use hylan G F 20 (Synvisc®/Synvisc One®) and sorbitol stabilised HA (Synolis™ VA), delivered via a single, carefully placed intra articular injection. Some patients feel a steady improvement over two to six weeks with relief that can extend towards six months. The evidence is mixed. A large meta analysis found small average pain benefits over placebo and flagged a higher rate of serious adverse events in pooled analyses, which is why many guidelines are cautious about routine HA. Yet individual responses vary and certain preparations remain widely used; in clinic I make space for that nuance and decide case by case.
Platelet rich plasma (PRP)
PRP is your own concentrated platelets, prepared the same day, aiming to deliver a pulse of growth factors into the joint. On average, published comparisons increasingly show PRP outperforming hyaluronic acid and corticosteroid for pain and function at three to twelve months, especially when leukocyte poor PRP and multi injection protocols are used. At the same time, one of the largest sham controlled trials reported no advantage of PRP over saline at twelve months, a reminder that technique, preparation and patient selection matter. My practice response to this split evidence is straightforward: I do not mix PRP with steroid in the same treatment cycle because preclinical and translational work suggests steroid can blunt the cellular signalling we are trying to harness. I standardise the PRP preparation and match the protocol to your goals and OA grade. In responders, improvements usually emerge over four to eight weeks and can last six to twelve months. In Singapore, PRP may be self funded or claimed under your hospital insurance with MediSave, depending on the care setting and your policy; we confirm this before booking.
PRP plus hyaluronic acid
There is a combination strategy—PRP plus hyaluronic acid—for selected knees. Recent evidence, including network meta analysis and newer randomised data, suggests the combination can equal or even outperform PRP alone for symptom relief in knee osteoarthritis, although results vary by product and protocol. I reserve this approach for patients whose goals and imaging profile suggest they would benefit from both a lubrication and a biologic signal in the same cycle.
Bone marrow aspirate concentrate (BMAC)
BMAC is a regenerative option that we discuss candidly. A landmark placebo controlled trial found no superiority over saline through six months, and technology overviews from orthopaedic groups describe a still uncertain evidence base. BMAC may have a role in carefully selected patients prepared for close follow up, but I present it as emerging rather than established. In Singapore, it may be self funded or claimed under hospital insurance with MediSave depending on how the procedure is billed and your individual policy; we check your eligibility in advance.
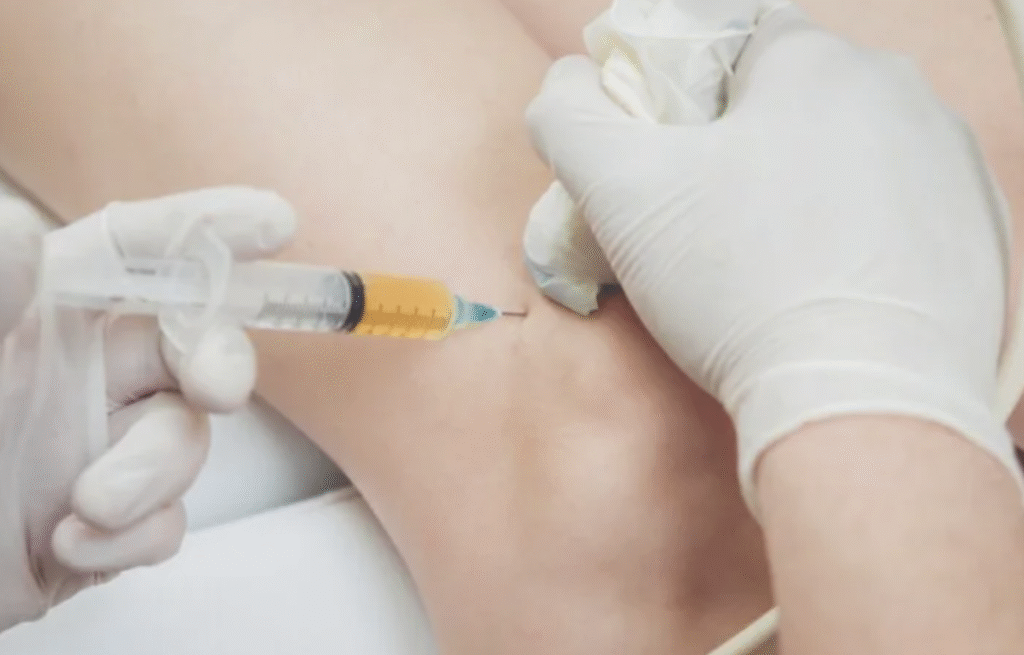
How I perform the procedure
Procedural details matter for both comfort and safety. I use a sterile, day surgery level setup in Singapore, with chlorhexidine or iodine skin prep and draping. The approach is typically an anterolateral, landmark guided injection. Landmark technique keeps costs down and is highly accurate in routine knees. When anatomy is altered by prior surgery, when there is a large effusion to aspirate first, or when precision into the suprapatellar pouch will clearly add value, I use ultrasound guidance. Evidence shows ultrasound improves needle placement accuracy and, in some contexts, patient reported outcomes. I numb the skin and joint lining with a small amount of local anaesthetic, aspirate if the joint is tight, and then make a single, smooth pass into the joint. Afterward you can walk out; most people return to everyday activity straight away and to sport in about a week if comfortable.
What to expect after an injection
Timelines vary by modality. Steroid acts fastest, often within days. Hyaluronic acid usually builds over two to six weeks. PRP tends to declare itself between four and eight weeks. BMAC—when used—generally takes longer. In my cohort of appropriately selected patients, roughly four out of five report meaningful improvement in pain and function by six to twelve weeks, and many enjoy a six to nine month easier movement window before we reassess. These numbers are averages; your knee and your goals are unique.
Safety and how we minimise risks
Safety is excellent when we are disciplined about sterile technique and selection. The most common issue is short lived soreness or a post injection inflammatory flare that settles with ice, rest and simple analgesics. Vasovagal fainting is uncommon and we prevent it with calm pacing, positioning and hydration. True joint infection is rare but is the complication we treat with the greatest respect, hence the scrub, the drape and the no shortcuts culture. For people with diabetes, corticosteroid can trigger a transient rise in blood glucose for two to three days; we discuss that risk beforehand and monitor. I avoid injections in the presence of active skin or joint infection, poorly controlled diabetes or compromised skin at the injection site, and I proceed cautiously and personally when patients are on anticoagulants.
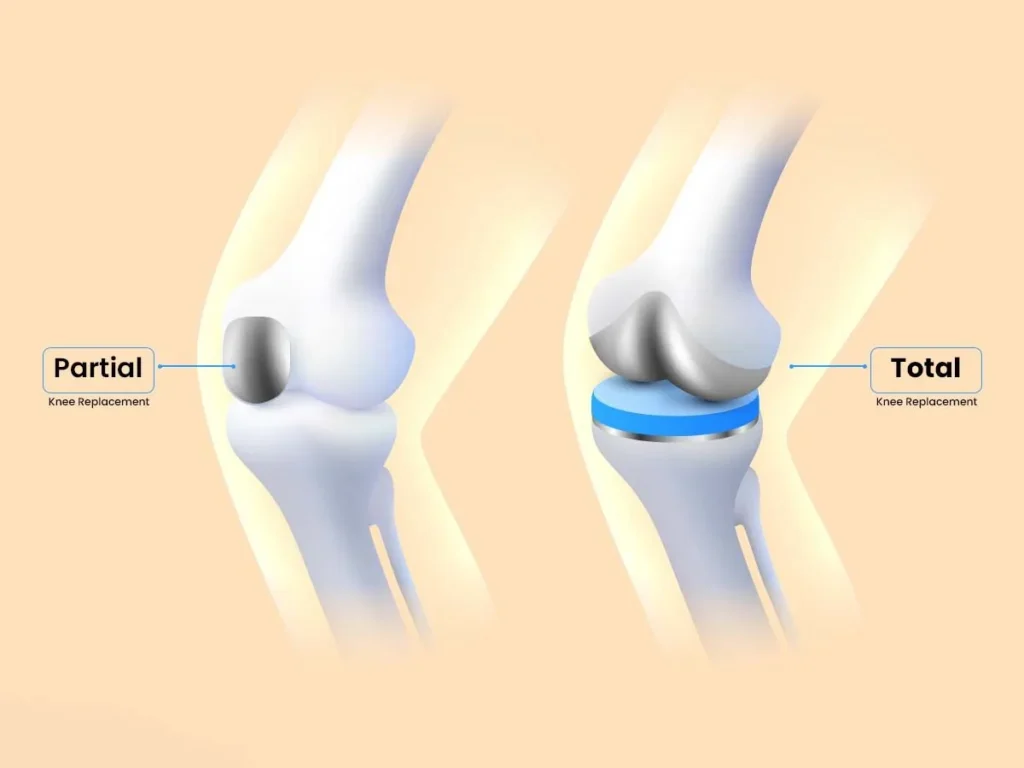
Timing around knee replacement surgery
If you are considering a total knee replacement, we plan injections with an eye to infection risk. Several analyses suggest that intra articular injections close to arthroplasty—particularly within about three months—are associated with a higher risk of postoperative infection, and newer data specifically implicate hyaluronic acid administered within the two months before surgery. Because the signal looks time dependent and patient specific, my standard advice in Singapore is to avoid injections within three months of planned arthroplasty and to coordinate with your surgeon.
Two real world cases from The Clifford Clinic
It may help to put these ideas into context. A 65 year old gentleman with long standing right sided osteoarthritis came in because stairs had become decisive: up meant pain, and pain meant avoidance. After assessment and imaging, we chose a PRP plus hyaluronic acid cycle using our landmark anterolateral approach in a sterile day surgery environment. He began gentle physiotherapy within forty-eight hours. By week six, he could ambulate without pain; by week twelve, he was back to hill walking; and at six months, he remained comfortable with a home programme and periodic check-ins.
In another case, a 60-year-old active woman with grade 2 osteoarthritis had not progressed on medication alone. We again selected PRP with hyaluronic acid, paired with closed-chain strengthening and footwear tweaks. She reported steady improvement at six, twelve and twenty four weeks and returned to doubles tennis with a clearer plan for quadriceps and hip work. These are not guarantees but illustrations of how we pair the window an injection gives with the work that makes it last.
Common questions in Singapore
Patients naturally ask about coverage, comfort and durability. In Singapore, the cost can be self funded or claimed under your hospital insurance with MediSave, depending on your individual plan and the care setting. We provide itemised documentation and confirm your eligibility with the hospital and your insurer before scheduling. The procedure itself is typically described as pressure rather than pain because we use local anaesthetic and a deliberate, single pass technique; ultrasound is available where it materially adds accuracy or comfort. Relief lasts different lengths for different knees; in my practice, six to nine months is common, sometimes longer with PRP or certain HAs. No injection reverses osteoarthritis. Steroid is not disease-modifying and, if overused, can be counterproductive for cartilage. PRP is the most intriguing biologic option but is not yet a proven disease modifier. Injections do not repair a degenerative meniscus, but they can quiet a painful, osteoarthritic knee with a degenerative tear so you can strengthen and move again.
Costs and access in Singapore
For transparency, pricing for an intra articular knee injection in my clinic starts from S$1,500 per knee, including sterile day surgery setup and follow up. Funding in Singapore is either self pay or claims under your hospital insurance with part of the bill paid via MediSave. Eligibility depends on your policy and how the procedure is billed (for example, as day surgery at an accredited facility). If the injection is performed purely as an outpatient clinic procedure without hospital billing, claims may not apply and the cost is self funded. We check all of this with you in advance so there are no surprises.
Rehabilitation and the long term plan
Technique matters, but what you do after the jab matters more. We default to early, joint friendly physiotherapy with an emphasis on closed chain strengthening, hip and core control, balance and progressive loading. For footwear, orthotics and gait tweaks, I often involve a podiatrist. When metabolic health or weight management is part of the picture, I can coordinate that plan as well. The aim is to convert pain relief into better mechanics, stronger tissue and renewed confidence so you need fewer procedures over time, not more.
Regulatory note for Singapore
Intra articular corticosteroids and hyaluronic acids are conventional therapies with established product labelling. PRP and BMAC are clinician directed, same day procedures using your own cells and blood components. Oversight of health products in Singapore sits with the Health Sciences Authority (HSA), and the governance of cell and tissue based therapies continues to evolve. In practice, that means we consent carefully, set expectations humbly and anchor decisions in evidence plus your goals.
If you are reading this in Singapore and knee pain is pushing you to move less and worry more, I would be glad to help you think it through. We will confirm the diagnosis, align on your goals and choose the least invasive plan that gets you moving again—whether that is physiotherapy only or a targeted injection paired with a clear rehabilitation path. Book a consult, bring your questions, and we will decide together.
Click here to schedule an appointment.
Important: This article is general information for the public in Singapore and does not replace a consultation. Discuss personal risks, benefits and alternatives with your clinician, especially if you have diabetes, are on blood thinners, or are planning knee replacement surgery.
References
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care & Research. 2020;72(2):149 162.
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Knee (Non Arthroplasty). Evidence Based Clinical Practice Guideline (3rd ed.). 2021.
- Pereira TV, Porfírio GJM, Naci H, et al. Viscosupplementation for knee osteoarthritis: systematic review and meta analysis. BMJ. 2022;378:e069722.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017;317(19):1967 1975.
- Qiao X, Ni S, Hu Z, et al. Efficacy and safety of corticosteroids, hyaluronic acid and platelet rich plasma for knee osteoarthritis: a Bayesian network meta analysis of RCTs. BMC Musculoskeletal Disorders. 2023;24:789.
- Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra articular Platelet Rich Plasma vs Placebo on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2021;326(20):2021 2030.
- Fang WH, Chiang ER, Chen KH, et al. Ultrasound Guided Knee Injections Are More Accurate Than Blind Injections: A Systematic Review of Randomized Controlled Trials. Arthroscopy, Sports Medicine, and Rehabilitation. 2021;3(4):e1289 e1302.
- Oo WM, McWilliams DF, Walsh DA. Comparison of ultrasound guidance with landmark guidance for intra articular knee injections: a narrative review. Australasian Journal of Ultrasound in Medicine. 2024.
- Larghi MM, Filmann N, Schipper I, et al. Septic arthritis following joint injections: a critical review. European Review for Medical and Pharmacological Sciences. 2022;26(3):1001 1013.
- Kim YM, Joo YB, Song J H. Preoperative intra articular steroid injections within 3 months increase the risk of periprosthetic joint infection in total knee arthroplasty: a systematic review and meta analysis. Journal of Orthopaedic Surgery and Research. 2023;18:148.
- Jones CM, Acuña AJ, Forlenza EM, et al. Hyaluronic acid injections administered within two months prior to total knee arthroplasty increase the risk for periprosthetic joint infection. Knee. 2025;53:103 107.
- Sanofi. SYNVISC® (hylan G F 20) Prescribing Information. Accessed 2025.
- Aptissen SA. Synolis™ VA Product Monograph. 2022.
- Shapiro SA, Kazmerchak SE, Heckman MG, Zubair AC, O’Connor MI. A Prospective, Single Blind, Placebo Controlled Trial of Bone
- Marrow Aspirate Concentrate for Knee Osteoarthritis. American Journal of Sports Medicine. 2017;45(1):82 90.
- American Academy of Orthopaedic Surgeons. Technology Overview: Concentrated Bone Marrow Aspirate for Knee Osteoarthritis. 2021.
- CPF Board (Singapore). Using MediSave for hospitalisation (including day surgery) and What MediShield Life covers you for. Accessed 2025.



No Comments