Unstable Kneecap Injury (Patellar Instability/Subluxation)

Understanding the Condition
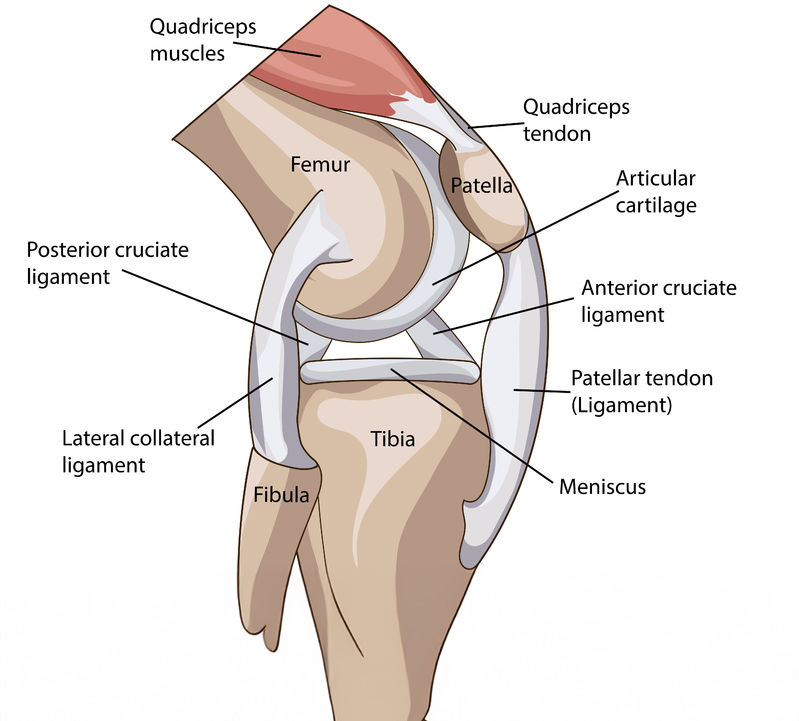
An unstable kneecap—also referred to as patellar instability or subluxation—occurs when the kneecap (patella) partially or completely moves out of its usual position in the trochlear groove of the thighbone (femur).
This misalignment often results in pain, discomfort, and a sense of instability during movement. In contrast to a full dislocation—where the patella completely exits its groove—a subluxation involves a partial shift before the bone returns to place.
Patellar instability can occur at varying degrees:
- Objective instability: One or more actual subluxation events have occurred.
- Potential instability: No history of subluxation, but structural risk factors are present.
- Patellofemoral pain syndrome: Pain without clear instability
Anatomy of the Patellar Tendon
The patellar tendon emerges as a continuation of the quadriceps tendon, passing beneath the kneecap before attaching to the tibial tuberosity. This arrangement acts like a spring, storing and releasing energy during powerful movements such as jumping and landing.
Key structures involved:
- Quadriceps muscle group: generates force to extend the knee
- Patella (kneecap): improves leverage and force transmission
- Patellar tendon: transfers force to the shin
- Infrapatellar bursae and Hoffa’s fat pad: help reduce friction and cushion underlying bone structures

What Causes Patellar Instability?
Multiple anatomical and traumatic factors contribute, including:
- Trauma: Direct blows or twisting injuries from sports or falls are common initiators
- Trochlear dysplasia: A shallow or malformed femoral groove fails to stabilize the patella
- Patella alta: A high-riding kneecap impedes proper tracking .
- Increased TT-TG distance: Abnormal alignment of the tibial tubercle increases lateral pull
- Ligament and muscular laxity: Loose connective tissues or weak vastus medialis obliquus (VMO) muscles destabilize knee mechanics
- Q-angle abnormalities: Knock-knee alignment increases lateral tracking forces
- Joint hypermobility: Conditions like Ehlers–Danlos syndrome elevate risk
Recognising the Symptoms
Common symptoms include:
- A sensation of the knee giving way, slipping or “sliding”.
- Audible popping or clicking as the patella shifts.
- Pain focused at the front of the knee, especially when using stairs, squatting or standing.
- Swelling, tenderness, and stiffness following a subluxation event.
- Locking sensations or catching during motion.
- Visible deformity might be present in severe or recurrent cases.

How We Diagnose It
1.History & Physical Exam
Discussions about trauma, activity, and recurrent sensations, paired with examinations like the apprehension test and assessing patellar tracking and muscle strength
2.Imaging Tests
- X-rays to assess bone alignment, patellar position, and trochlear depth
- MRI for detailed evaluation of soft tissue injuries (MPFL, cartilage damage) after initial imaging or recurrent episodes
- CT scans may be used to accurately measure TT-TG distance or bone alignment.
3.Diagnostic Arthroscopy
Sometimes used in operating theatre to directly visualize joint structures and assess damage artisanorthopaedics.sg.
Types of treatments
RICE: Managing Knee Pain and Swelling
RICE stands for Rest, Ice, Compression, and Elevation—a simple and effective way to manage pain and swelling in knee.
Rest
Avoid activities that strain the knee, such as jumping or squatting. Use relative rest—gentle movement is okay, but avoid anything painful.
Ice
Apply an ice pack to the front of the knee for 15–20 minutes every 2–3 hours, especially during flare-ups. This helps reduce swelling and numbs pain. Always wrap the ice—don’t apply directly to skin.
Compression
Use a knee sleeve or elastic bandage to reduce swelling and support the joint. Make sure it’s snug but not too tight.
Elevation
Prop your leg up on pillows so your knee is above heart level. This helps drain fluid and reduce pressure in the joint.


💊 Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs such as ibuprofen, naproxen, or diclofenac are commonly prescribed or recommended to manage inflammation and relieve pain after a kneecap subluxation. When the patella shifts out of alignment, surrounding tissues—such as the synovium, ligaments, or cartilage—can become irritated or swollen. NSAIDs work by inhibiting enzymes involved in the production of prostaglandins, which are substances that cause inflammation and pain in the body.
These medications can help reduce:
- Acute swelling in the knee joint
- Localized heat and tenderness
- Discomfort during movement or rest
While effective in the short term, NSAIDs should be used with guidance from a doctor, particularly in individuals with a history of gastrointestinal, kidney, or cardiovascular issues.
Bracing or Taping to Support Alignment
A patellar-tracking knee brace or rigid sleeve is often recommended to maintain proper alignment of the kneecap during healing. These braces are specifically designed to prevent the patella from drifting laterally (to the outside of the knee), which is the most common direction of subluxation. They also provide mechanical feedback that encourages proper movement patterns.
Additionally, taping techniques like McConnell or kinesiology taping can:
- Reduce pain by limiting patellar glide
- Improve proprioception (body awareness)
- Assist muscle activation, particularly of the vastus medialis obliquus (VMO) muscle, which helps stabilize the kneecap
These external supports are especially useful during the early recovery phase and when returning to activity or sport.


Crutches or Walking Aids
Following a subluxation event, weight-bearing may cause pain, instability, or further stress on healing tissues. Using crutches or a walking aid temporarily can help:
- Offload pressure from the affected knee
- Reduce risk of further injury from buckling or giving way
- Encourage healing by preventing overuse during the acute phase
- Crutches are typically used for a few days to a week, depending on pain levels and swelling. As mobility improves, patients gradually transition back to full weight-bearing, often while wearing a brace or undergoing physiotherapy.
When Is Surgery Needed?
Surgical intervention may be considered if:
- Subluxations are recurrent or severe despite conservative management
- There’s documented injury to medial patellofemoral ligament (MPFL) or joint cartilage
- Underlying bone or alignment issues (trochlear dysplasia, patella alta, altered TT-TG) require correction
Why Choose Clifford Orthopaedics?
Our Orthopaedic specialists, trained in the latest ultrasound- and arthroscopy-guided techniques, provide accurate diagnosis and personalised treatment plans.
We emphasise conservative care like tailored physiotherapy, bracing, and movement retraining. When surgery is needed, we utilise effective procedures such as MPFL reconstruction and realignment osteotomy, ensuring minimally invasive techniques and faster rehabilitation.
Our Services
EFFECTIVE SOLUTIONS
Facing persistent knee pain? Take control of your mobility and comfort—schedule your consultation today and begin your journey towards relief with personalized, expert care.