Patellar Tendinopathy (Jumper’s Knee):
A Comprehensive Guide
What Is Patellar Tendinopathy?
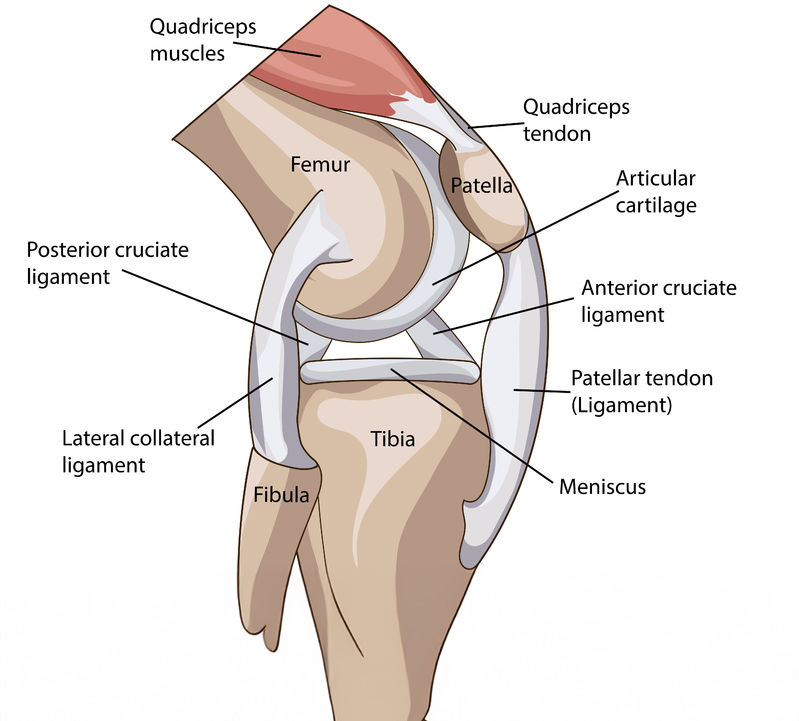
Patellar tendinopathy, often called jumper’s knee, is a condition affecting the tendon that connects your kneecap (patella) to your shin bone (tibia). This tendon acts as a critical link in your knee extensor mechanism—transferring the force generated by your quadriceps muscle to straighten your knee .
Patellar tendinopathy can manifest in two primary forms:
- Tendonitis: inflammation of the tendon tissue
- Tendinosis: microscopic degeneration and microtears in the tendon, without significant inflammation
It typically occurs at the tendon’s lower patellar attachment (inferior pole) and is particularly common among athletes involved in jumping and running sports
Anatomy of the Patellar Tendon
The patellar tendon emerges as a continuation of the quadriceps tendon, passing beneath the kneecap before attaching to the tibial tuberosity. This arrangement acts like a spring, storing and releasing energy during powerful movements such as jumping and landing.
Key structures involved:
- Quadriceps muscle group: generates force to extend the knee
- Patella (kneecap): improves leverage and force transmission
- Patellar tendon: transfers force to the shin
- Infrapatellar bursae and Hoffa’s fat pad: help reduce friction and cushion underlying bone structures
What Causes It?
Patellar tendinopathy is a gradual condition, usually caused by:
Repetitive microtrauma from jumping, running, frequent deceleration or acceleration, and sudden impacts
Excessive load on the tendon that exceeds its ability to adapt, leading to microtears and degeneration
Structural change within the tendon over time—thickening, uneven texture, and neo-vascular ingrowth
Common Risk Factors
- High-impact sports: basketball, volleyball, soccer, running, gymnastics, track & field
- Muscle imbalances: tight quadriceps, hamstrings, ITB, or weak gluteus medius/quadriceps
- Biomechanical issues: flat or high-arched feet, abnormal patellar tracking, knock knees, improper technique
- Sudden workload spikes: rapid increase in training frequency, intensity, surface changes, or switching sports
- Footwear and surfaces: inadequate cushioning or training on hard surfaces increases stress
Signs & Symptoms
Recognising the warning signs early helps prevent chronic degeneration. Common clinical features include:
- Pain just below the kneecap, worsened by jumping, squatting, running, or stairs
- Tendon tenderness on palpation at the inferior patellar pole
- Morning stiffness in the tendon or knee joint
- Tendon thickening or swelling compared to the opposite side
- Tightness or pain during knee bending, squatting, jumping, or jogging
- Weakness or reduced performance, especially during explosive movements
Despite activity-related pain, rest may not immediately alleviate symptoms due to underlying structural changes .

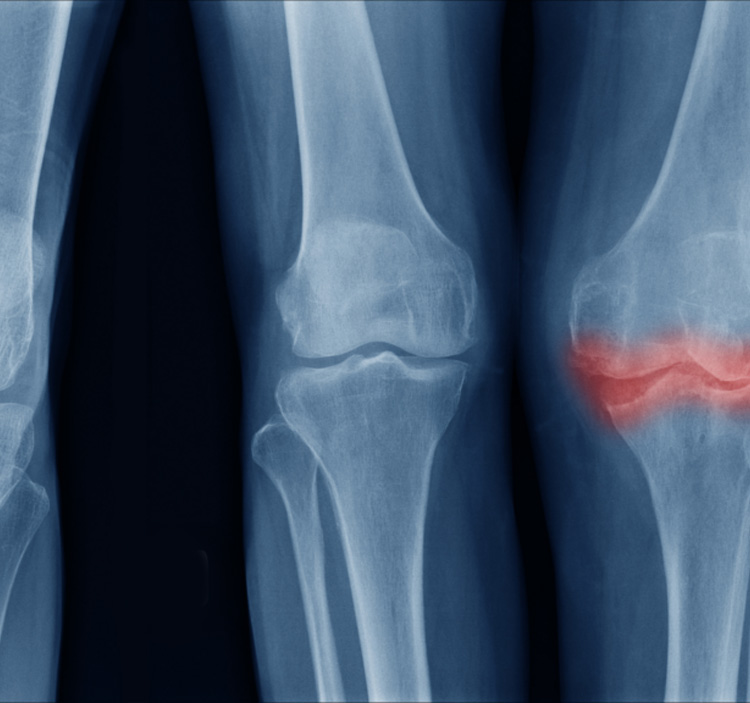
How We Diagnose It?
A structured assessment is important for accurate diagnosis:
Clinical exam: evaluates pain location, range of motion, tenderness, strength, and functional load tolerance.
Movement tests: pain during squats, single-leg hopping, stair decline, and kneeling
Imaging (if needed):
- Ultrasound: reveals tendon thickening, altered structure, neovascularization
- MRI: detects microtears, intratendinous degeneration
- X-ray: generally unhelpful unless other bone pathologies are suspected
Types of treatments
RICE: Managing Knee Pain and Swelling
RICE stands for Rest, Ice, Compression, and Elevation—a simple and effective way to manage pain and swelling in knee conditions like patellar tendinopathy.
Rest
Avoid activities that strain the knee, such as jumping or squatting. Use relative rest—gentle movement is okay, but avoid anything painful.
Ice
Apply an ice pack to the front of the knee for 15–20 minutes every 2–3 hours, especially during flare-ups. This helps reduce swelling and numbs pain. Always wrap the ice—don’t apply directly to skin.
Compression
Use a knee sleeve or elastic bandage to reduce swelling and support the joint. Make sure it’s snug but not too tight.
Elevation
Prop your leg up on pillows so your knee is above heart level. This helps drain fluid and reduce pressure in the joint.


RegenPRP® Therapy for Patellar Tendinopathy
When conservative treatments like RICE and physiotherapy don’t provide lasting relief, RegenPRP® (Platelet-Rich Plasma) offers a powerful regenerative solution.
RegenPRP® is an advanced therapy that uses your own blood to promote natural tendon healing. A small blood sample is drawn and processed using a Swiss-engineered RegenKit® system to extract platelet-rich plasma, which is rich in growth factors.
These growth factors:
- Stimulate tissue repair
- Encourage new collagen production
- Reduce inflammation at the tendon site
💉 How Is It Done?
- Step 1: Your blood is drawn and spun in a special centrifuge.
- Step 2: The concentrated PRP is injected precisely into the affected tendon under ultrasound guidance.
- Step 3: You follow a guided rehab plan to support tendon regeneration.
✅ Benefits of RegenPRP®
- Addresses the root cause (tendon degeneration), not just symptoms
- Minimally invasive and done in-clinic
- Uses your own cells—no synthetic drugs or risk of allergy
- Proven improvements in pain, stiffness, and function over weeks to months
- Suitable for chronic or stubborn tendinopathy unresponsive to rest and physiotherapy.
Foot Orthotics: A Customised Solution
Your feet form the foundation of movement, and poor foot alignment can create stress that travels upward—placing extra strain on your knees, hips, and tendons. In patellar tendinopathy, even slight biomechanical imbalances in the feet can worsen tendon loading during walking, running, or jumping.
For example:
- Flat feet (overpronation) cause inward knee collapse, increasing tension on the patellar tendon
- High arches (supination) reduce shock absorption, concentrating impact on the knees
- Uneven leg lengths or abnormal foot angles can shift forces unevenly, overloading one knee more than the other
🦶 Benefits of Foot Orthotics
- Corrects alignment (e.g. overpronation/supination)
- Redistributes pressure across the foot
- Reduces tendon overload by improving lower limb biomechanics
- May be custom-made or off-the-shelf, based on your needs
👟 Choosing Proper Footwear
- Look for shoes that offer:
- Good arch support
- Shock-absorbing soles
- Heel and ankle stability

When Is Surgery Considered?
Surgery becomes an option if symptoms persist despite optimized conservative care for 6–12 months:
- Tendon debridement to remove degenerated tissue
- Tear repair for partial or complete tendon ruptures
Recovery includes immobilization, gradual physiotherapy, and functional rehab.
Why Choose Clifford Orthopaedics?
We deliver comprehensive, evidence-based care tailored to your condition and lifestyle:
- Multidisciplinary assessment: orthopaedic evaluation, physiotherapy, imaging support
- Individualised rehab planning: carefully staged loading supported by skilled physiotherapists
- Access to advanced treatments: extracorporeal shockwave therapy, guided injections when required
- Focused on long-term joint health: prevention, education, and movement re-education
Our Services
EFFECTIVE SOLUTIONS
Facing persistent knee pain? Take control of your mobility and comfort—schedule your consultation today and begin your journey towards relief with personalized, expert care.