
12 Nov PRP Knee Injections for Osteoarthritis in Singapore: A 2025 Evidence‑Based Guide to PRP, Hyaluronic Acid, and PRP+HA
Introduction
If you are searching for PRP knee injection Singapore because knee osteoarthritis is making mornings stiff, stairs painful and squatting difficult, you are not alone. Many people in Singapore are comparing platelet‑rich plasma (PRP), hyaluronic acid (“knee gel”), and combination PRP + HA to reduce pain, improve function, and delay surgery. This long‑form guide explains, in plain language, what a PRP knee injection is, how it compares with hyaluronic acid knee injection, why a combined approach is sometimes chosen, how many injections are typically required, how long results last, whether the treatment is safe, what the typical out‑of‑pocket costs look like locally, and how to choose a clinician. It is written for patients and families who want an evidence‑based overview, and it cites high‑tier research and Singapore health resources in the reference list at the end.
Throughout, Dr Gerard Ee is described as a Singapore‑based doctor with a special interest in orthopaedics and knee pain, and his peer‑reviewed publications are included to demonstrate clinical credibility.
What is PRP for knee osteoarthritis, and how does a PRP knee injection work?
PRP is prepared from your own blood by concentrating platelets that carry growth factors and anti‑inflammatory mediators. When this concentrated solution is injected into a symptomatic knee joint, the goal is to reduce inflammatory signalling within the joint and to nudge the local environment toward healing. Because the product is autologous—meaning it comes from you—systemic allergic reactions are uncommon, and the most frequent post‑injection experiences are transient soreness or fullness that settle over a few days. Professional organisations first described PRP as a promising but evolving therapy several years ago; since then, additional randomised trials and meta‑analyses have expanded the dataset and clarified where PRP sits alongside hyaluronic acid and corticosteroid injections in non‑operative care.
Is PRP better than hyaluronic acid for knee osteoarthritis?
Many patients arrive with this exact question, and recent comparative reviews help to answer it. Across multiple contemporary meta‑analyses, PRP frequently shows larger improvements in pain and function than hyaluronic acid at mid‑term follow‑up, especially around the six‑ to twelve‑month mark. These findings are not uniform in every publication because protocols, PRP preparations and OA severity vary; however, the trend across the newer literature has moved in favour of PRP for many symptomatic patients who wish to remain active and postpone arthroplasty. It is equally important to point out that at least one well‑designed randomised trial published in 2021 found no advantage of PRP over placebo in its protocol. That trial is a useful reminder that details such as platelet dose, the presence or absence of leukocytes, and the number and spacing of injections can influence outcomes. The practical upshot is that a personalised consultation remains essential, and the “better” option for you depends on your OA grade, alignment, activity goals and tolerance for medications.
Can PRP and hyaluronic acid be combined, and who benefits from PRP + HA?
Combination therapy is increasingly discussed in Singapore because many people want the best chance of sustained relief without surgery. Recent systematic reviews and meta‑analyses indicate that PRP combined with hyaluronic acid is safe and, for carefully selected patients, can deliver equal or superior pain and functional improvements compared with PRP alone at six to twelve months. Some studies also describe potential structural signals—such as changes in bone‑marrow oedema on MRI—when PRP is added to HA, although definitive disease‑modifying claims would be premature. In practice, surgeons either administer both in one session or stage them over weeks, depending on OA severity, effusions, and patient goals. This choice is best made after reviewing your X‑rays and, when appropriate, your MRI.
How many PRP knee injections will I need, and how long do results last?
The number of injections matters. Evidence comparing one versus multiple PRP injections shows that a series is often more effective than a single dose, with three injections spaced two to four weeks apart commonly used in studies and in clinics. Several trials and reviews demonstrate that three or even five injections produce greater improvements than one, and that three and five injections often perform similarly by one year, which makes a three‑shot plan a practical balance between benefit and convenience for many patients. Durability also matters, and many programmes report results that build over two to six weeks, peak around three to six months, and persist toward the twelve‑month mark. Patients in Singapore often repeat injections when symptoms recur, typically within six to twelve months, based on shared decision‑making and their activity calendar.
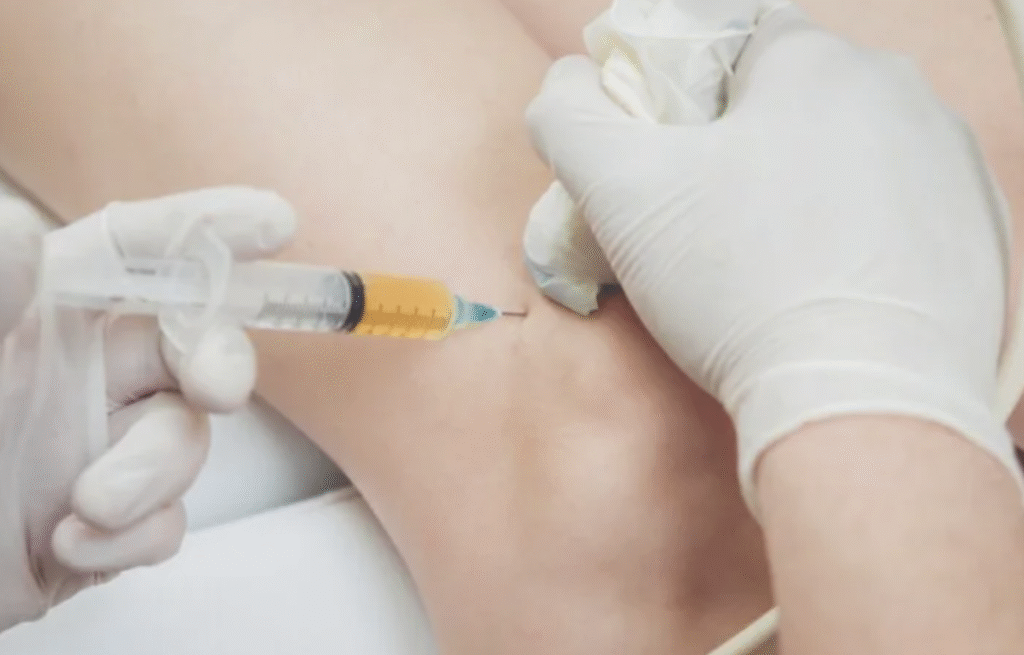
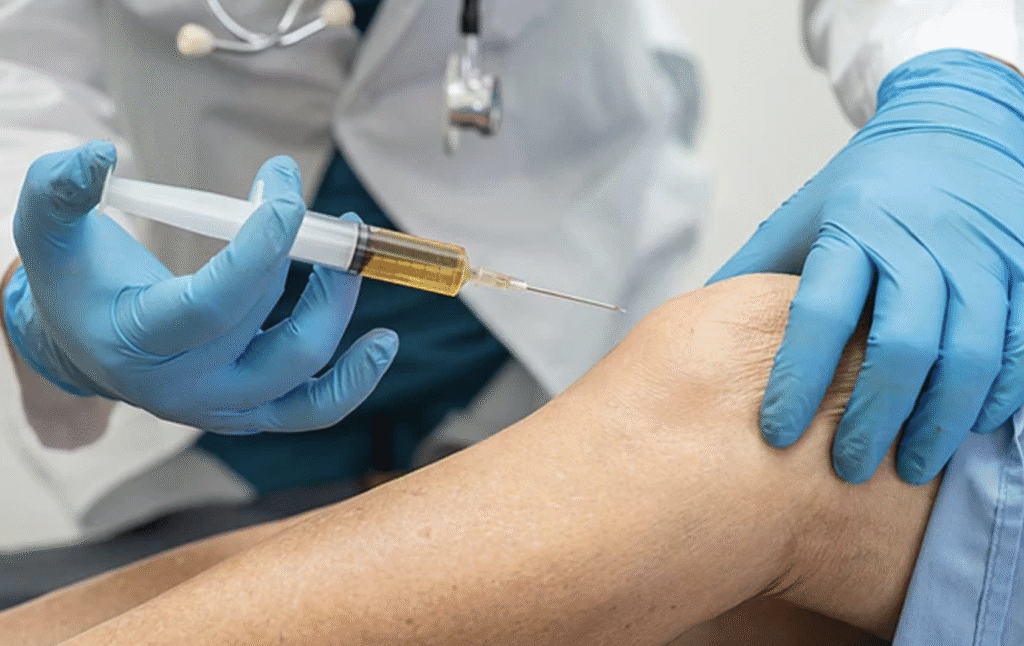
What happens during an ultrasound‑guided PRP knee injection in Singapore?
A modern PRP knee injection is an outpatient procedure delivered under ultrasound guidance. After a small blood draw, the sample is processed to produce PRP—commonly a leukocyte‑poor formulation if tolerability is a priority. The surgeon then uses ultrasound to visualise the suprapatellar recess or another appropriate compartment and guides the needle into the joint while watching the tip in real time.
Ultrasound improves accuracy across the common portals compared with landmark‑guided techniques and allows the team to adapt to synovitis, effusions or osteophytes. Many protocols minimise or avoid intra‑articular local anaesthetic because of laboratory evidence that some anaesthetics can be chondrotoxic and because certain agents may reduce platelet activity. Comfort is still carefully managed, usually with topical anaesthetic, peri‑capsular local anaesthetic or other measures decided during your consult.
Is PRP safe, and how does it compare to long‑term painkillers?
PRP’s safety profile is favourable in appropriately selected patients. Because the injectate is autologous, allergic reactions are rare, and the most common immediate effects are temporary soreness, a sense of fullness, or low‑grade swelling that resolves with activity modification. Large comparative analyses report adverse‑event rates similar to or lower than those of other common injectables. Safety should also be assessed in the context of alternatives. Long‑term use of non‑steroidal anti‑inflammatory drugs (NSAIDs) is associated with stomach irritation and peptic ulcer disease; Singapore health resources advise that NSAIDs be used at the lowest effective dose for the shortest possible time and list gastric complications among the recognised risks. For many patients who have already experienced gastric pain on tablets, local therapies such as PRP, hyaluronic acid or both offer a way to reduce pill burden while addressing knee pain.
Should I stop anti‑inflammatory tablets before a PRP knee injection?
Many protocols recommend avoiding nonselective NSAIDs and aspirin for a short window before and after PRP because these medications can blunt platelet activity. There is also an ongoing discussion about the type and amount of local anaesthetic used around the joint; basic science and translational studies caution against direct intra‑articular exposure to certain anaesthetics because of potential chondrotoxicity. In Singapore, surgeons typically provide a written plan that preserves PRP biology while keeping the procedure comfortable, often substituting paracetamol for NSAIDs during this brief period.
How much do PRP knee injections cost in Singapore, and is MediSave applicable?
Because PRP for knee osteoarthritis is usually performed in private outpatient settings, published fees vary with the PRP preparation system, whether ultrasound guidance is used, and whether you are having a single injection or a short series. Publicly accessible clinic pages in Singapore commonly cite figures in the lower four‑digit range per session, and several specialist pages describe a broader span from several hundred to a few thousand dollars per injection depending on the joint and protocol. For hyaluronic acid knee injections, Singapore clinic pages frequently note that viscosupplementation is generally not MediSave‑claimable as an outpatient procedure, although selected private insurance plans may offer partial benefits depending on policy and indications. Because pricing and coverage change, the most reliable figure is the written quotation you receive after consultation, but these published ranges are useful for initial budgeting.
Real patient example: how did a 55‑year‑old in Singapore respond to PRP + HA?
An anonymised case illustrates how these timelines play out in real life. A 55‑year‑old female presented with right knee pain that was worse in the mornings and severe enough to prevent squatting. She had tried oral anti‑inflammatories but developed gastric pain after repeated use, which made long‑term medication unattractive. Her X‑ray showed osteoarthritic changes consistent with symptomatic degeneration. After a thorough discussion about PRP, hyaluronic acid and the evidence for combined therapy, she underwent an ultrasound‑guided intra‑articular injection plan that combined PRP with a hyaluronic acid viscosupplement. Two weeks later, she reported significant pain relief and was walking without discomfort. Follow‑up at two months, four months, six months and nine months confirmed persistent improvement. She now repeats the injection approximately every nine months when symptoms begin to return. For readers who want to visualise typical radiographic changes, you can view an illustrative anonymised knee osteoarthritis X‑ray here: download the sample X‑ray; the image shows joint‑space narrowing and osteophyte formation.
Who should consider PRP, HA or PRP + HA for knee osteoarthritis?
People with mild‑to‑moderate osteoarthritis who want to walk farther, manage stairs, or return to low‑impact activity without escalating tablets are commonly good candidates for PRP, HA or a combined approach. Individuals who cannot tolerate NSAIDs because of stomach irritation or ulcer history often prefer injections to reduce systemic side effects. Conversely, those with very advanced deformity, gross instability or active infection may be counselled toward different options. The best way to choose among PRP, HA and PRP+HA is to review your history, examination and imaging with a surgeon who can match evidence to your goals.
What does the latest evidence and guideline landscape say right now?
The American Academy of Orthopaedic Surgeons’ 2021 guideline described PRP as a therapy that may reduce pain and improve function in symptomatic knee osteoarthritis, reflecting the strength of evidence available at that time. Since then, comparative meta‑analyses and network meta‑analyses have strengthened support for PRP compared with hyaluronic acid and corticosteroids at six to twelve months in appropriately selected patients, and several have placed PRP—and in some models PRP + HA—at or near the top for pain relief and functional gains. At the same time, a rigorous placebo‑controlled randomised trial in 2021 reported no PRP advantage under its specific protocol, and studies continue to explore optimal dose, platelet counts and the role of leukocytes. The most responsible counselling therefore avoids sweeping claims and focuses on individualised treatment planning.
Why consider Dr Gerard Ee if I am exploring PRP knee injections in Singapore?
Outcomes with PRP and hyaluronic acid depend on the right patient, the right protocol and precise delivery. Dr Gerard Ee is a Singapore‑based doctor with a special interest in orthopaedics and knee pain whose peer‑reviewed publications demonstrate methodological rigour and attention to joint mechanics. His co‑authored paper in The Journal of Bone and Joint Surgery (American) reports a large epidemiological analysis in an Asian population, reflecting careful study design and statistical interpretation. His lead‑authored study in Clinical Orthopaedics and Related Research links minimally invasive spine surgery to lower surgical‑site infection rates compared with open approaches, underscoring a longstanding focus on safety. His work in The Knee explains the value of computer navigation for intra‑operative joint‑line measurement in total knee arthroplasty, a topic closely related to the biomechanics that biologic injections aim to support. This research background supports a clinical style that is data‑driven, ultrasound‑guided and centred on long‑term function for Singapore patients choosing non‑operative care.
How does a PRP knee injection compare with steroid injections, and do injectables change the disease?
Corticosteroid injections can provide rapid relief over weeks but tend to be shorter‑lived; PRP usually builds more gradually and often outperforms steroids at mid‑term checkpoints in comparative analyses. Hyaluronic acid is another alternative that can improve lubrication and shock absorption, with variable effect sizes versus placebo across products. Whether any injectable changes disease progression remains under investigation, and the most balanced counselling is careful not to promise cartilage growth or reversal of degeneration. Instead, injections should be framed as part of a broader programme—alongside strengthening, load management and weight optimisation when appropriate—to reduce pain, improve function and delay escalation.
What questions do patients in Singapore most often ask before booking?
Patients commonly ask how quickly they will feel better and when they can return to work. Most people resume desk work within a day or two after a PRP knee injection, while low‑impact activity is phased back during the first week and higher‑impact activity is reintroduced later according to symptoms and surgeon advice. Another frequent question concerns how many injections are needed, and the answer is that multi‑dose strategies tend to outperform single shots for many patients, with three injections a common plan that balances benefit and convenience. People also ask about cost and coverage, and the most accurate figure is the written quotation you receive after consultation; however, clinic pages in Singapore provide indicative ranges and often state that hyaluronic acid knee injections are usually not MediSave‑claimable in outpatient settings. Finally, patients want to know whether PRP or PRP + HA is “better,” and the honest answer is that the choice depends on your osteoarthritis grade, alignment, activity targets, and tolerance for tablets. A short conversation with imaging in hand is the fastest way to a personalised plan.
Conclusion
PRP knee injections, with or without hyaluronic acid, have become a mainstay non‑surgical option for osteoarthritis in Singapore. Contemporary evidence often places PRP ahead of hyaluronic acid and corticosteroids for pain and function at six to twelve months, and combination PRP + HA can provide additional benefit for selected patients who want durability without surgery. The anonymised case described here mirrors what many people experience: meaningful pain reduction within two weeks, sustained gains through nine months, and occasional repeat injections when symptoms return. Safety is favourable when the treatment is delivered by experienced hands under ultrasound guidance, and thoughtful aftercare that respects platelet biology helps maximise results. If you are comparing clinics for PRP knee injection Singapore, look beyond product names and consider the surgeon’s experience, image‑guided technique, protocol design and follow‑up structure. An evidence‑based consultation with a Singapore‑based doctor with a special interest in orthopaedics and knee pain, such as Dr Gerard Ee, provides the best platform for an informed, personalised plan that fits your goals, your imaging and your calendar.
This article is educational and does not replace a personalised medical consultation. Suitability for PRP, hyaluronic acid or combined therapy depends on individual assessment, imaging, goals and comorbidities.
References
- American Academy of Orthopaedic Surgeons. Platelet‑Rich Plasma (PRP) for Knee Osteoarthritis: Technology Overview (systematic review of studies through August 25, 2021). aaos.org
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Knee (Non‑Arthroplasty): Evidence‑Based Clinical Practice Guideline, adopted August 31, 2021. aaos.org
- Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra‑articular PRP vs Saline on Pain and Medial Tibial Cartilage Volume in Knee Osteoarthritis: Randomized Clinical Trial. JAMA, 2021. JAMA Network
- Xu H, et al. Comparison of hyaluronic acid and platelet‑rich plasma in knee osteoarthritis: meta‑analysis. 2025. PubMed
- Li YF, et al. Platelet‑Rich Plasma Is More Effective Than Hyaluronic Acid for Knee Osteoarthritis: Meta‑analysis of RCTs. Arthroscopy, 2025. arthroscopyjournal.org
- Gupta N, et al. Long‑term effectiveness of intra‑articular injectables in knee osteoarthritis: network meta‑analysis. J Orthop Surg Res, 2025. BioMed Central
- Khalid S, et al. Comparative effectiveness of intra‑articular therapies in knee osteoarthritis: meta‑analysis. 2023–2024. PMC+1
- Ivander G, et al. A comparison of intra‑articular hyaluronic acid and PRP for knee osteoarthritis: systematic review (concluding insufficient evidence for PRP superiority). Orthopedic Reviews, 2024. orthopedicreviews.openmedicalpublishing.org
- Du D, et al. Clinical efficacy of PRP plus hyaluronic acid vs PRP alone in knee osteoarthritis: meta‑analysis. J Orthop Surg Res, 2025. BioMed Central
- Liu Q, Ye H, Yang Y, Chen H. PRP combined with hyaluronic acid vs PRP alone for knee osteoarthritis: meta‑analysis. PLOS ONE, 2025. PLOS
- Sun SF, et al. Combined cross‑linked hyaluronic acid and PRP vs PRP alone for knee osteoarthritis: randomized trial. Scientific Reports, 2021. Nature
- Görmeli G, et al. Multiple PRP injections outperform single PRP and hyaluronic acid in early knee osteoarthritis: randomized, double‑blind, placebo‑controlled trial. Knee Surg Sports Traumatol Arthrosc, 2017. PubMed
- Zhuang W, et al. Single vs three vs five PRP injections for knee osteoarthritis: systematic review and study‑level meta‑analysis (three and five superior to one). J Orthop Surg Res, 2024. BioMed Central
- Fang WH, et al. Ultrasound‑guided knee injections are more accurate than landmark‑guided injections across portals. Arthroscopy Sports Med Rehab, 2021. arthroscopysportsmedicineandrehabilitation.org
- Kasitinon D, et al. Accuracy and efficacy of ultrasound‑guided vs landmark‑guided knee injections/aspirations: systematic review. 2025. PubMed
- Di Martino A, et al. Leukocyte‑rich vs leukocyte‑poor PRP for knee osteoarthritis: double‑blind randomized trial showed similar clinical outcomes at 12 months. Am J Sports Med, 2022. PubMed
- Xiong Y, et al. Meta‑analysis across osteoarthritis sites suggesting leukocyte‑poor PRP may have tolerability advantages. Frontiers in Medicine, 2023. Frontiers
- Bausset O, et al. Impact of local anaesthetics on platelet functionality: laboratory evidence relevant to PRP workflows. 2014. PMC
- Tognoloni A, et al. Chondrotoxicity of local anaesthetics and protective role of PRP: updated evidence. 2024. ScienceDirect
- Pirri C, et al. Chondrotoxicity of intra‑articular treatments with emphasis on local anaesthetics. 2024. MDPI
- HealthHub Singapore. Non‑steroidal anti‑inflammatory drugs (oral): patient guidance on stomach‑ulcer risk. HealthHub
- SingHealth. Peptic ulcer disease overview noting NSAIDs as a cause. singhealth.com.sg
- Apex Sports Clinic Singapore. PRP treatment in Singapore: typical cost range S$1,000–S$1,500. apexsportsclinic.sg
- Dr Andrew Dutton Orthopaedics. PRP injection in Singapore: cost typically ranges from several hundred to a few thousand dollars per injection. drandrewdutton.com
- Ray of Health. PRP treatment for knee in Singapore: typical per‑session cost range. Ray of Health
- Wonder Health. Hyaluronic acid knee injection in Singapore: outpatient treatment not MediSave‑claimable. wonderhealth.sg
- Apex Sports Clinic Singapore. Hyaluronic acid knee gel injection page noting non‑MediSave status for outpatient care and general payment guidance. apexsportsclinic.sg
- SingHealth. Patient information on PRP injection risks and precautions. singhealth.com.sg
- Mayo Clinic (professional news). Clinical experience summary indicating typical PRP relief windows of six to twelve months in knee osteoarthritis. Mayo Clinic
- Liu G, Tan JH, Ee G, et al. Morphology and Prevalence Study of Lumbar Scoliosis in 7,075 Multiracial Asian Adults. J Bone Joint Surg Am, 2016;98(15):1307‑12. PubMed
- Ee WWG, Lau WL, Yeo W, Yap VB, Yue WM. Does Minimally Invasive Surgery Have a Lower Risk of Surgical Site Infections Compared with Open Spinal Surgery? Clin Orthop Relat Res, 2014;472(6):1718‑24. PubMed
- Ee G, Pang HN, Chong HC, et al. Computer navigation is a useful intra‑operative tool for joint‑line measurement in total knee arthroplasty. The Knee, 2013;20(5):256–262 (online 2012). thekneejournal.com
- Ee GWW, Jiang L, Guo CM, et al. Comparison of Clinical Outcomes and Radiographic Measurements in Four Different Treatment Modalities for Osteoporotic Compression Fractures. J Spinal Disord Tech / Clinical Spine Surgery. PubMed+1
- Malhotra R, Ee G, Pang SY, Kumar N. A silent acute abdomen in a patient with spinal cord injury. BMJ Case Reports, 2013. casereports.bmj.com
- Sivasubramanian H, Ee G, Srinivasaiah MG, De SD. “Not Always a Baker’s Cyst” – Unusual central postero‑medial meniscal cyst. Open Orthopaedics Journal, 2012. openorthopaedicsjournal.com



No Comments